New Drug for Hard-to-Treat Colitis and Crohn's
Moderators: Rosie, Stanz, Jean, CAMary, moremuscle, JFR, Dee, xet, Peggy, Matthew, Gabes-Apg, grannyh, Gloria, Mars, starfire, Polly, Joefnh
- Tessa
- Rockhopper Penguin

- Posts: 774
- Joined: Thu May 26, 2005 2:49 pm
- Location: Málaga, Spain (Costa del Sol)
- Contact:
New Drug for Hard-to-Treat Colitis and Crohn's
Hi
Not sure if you have posted this already.
Just wanted to share it with you.
FDA OKs New Drug for Hard-to-Treat Colitis and Crohn's
Love,
Tessa
Not sure if you have posted this already.
Just wanted to share it with you.
FDA OKs New Drug for Hard-to-Treat Colitis and Crohn's
Love,
Tessa
DX Secondary Adrenal Insufficiency= Panhypopituitarism,POTS & MC. Anaphylactic reaction to foods & some drugs.
Gluten & Dairy free diet+hydrocortisone, Florinef, Sea Salt, Vit B Complex, Potassium, Sodium, Magnesium...
Gluten & Dairy free diet+hydrocortisone, Florinef, Sea Salt, Vit B Complex, Potassium, Sodium, Magnesium...
Hi Tessa,
As far as I'm aware, that's the first that we've seen about Entyvio (vedolizumab) on this discussion board. It's apparently a new class of drugs, as far as treating IBDs is concerned (it's an integrin receptor antagonist). It will be interesting to see how it fares in actual use.
IMO, the FDA should have waited before releasing it for use, based on their obvious concerns about the possible risk of patients developing progressive multifocal leukoencephalopathy (PML). Call me old-fashioned, but I believe that the FDA should be required to make sure that all trials are completed before a drug is released for sale, whenever there is a reason to suspect that a significant risk of adverse events exists. Apparently they chose to allow patients who receive prescriptions for the drug to be used as guinea pigs for determining or ruling out any risk of developing PML. That's clear in the FDA's requirement that the drug maker "must conduct a post-approval study to further investigate the risk of PML among patients taking Entyvio".
That said, this certainly isn't the first time that the FDA has approved a drug before the extent of risks have been verified by trials. They don't actually perform any tests themselves. Instead, they rely on the judgments of selected panel members (many/most of whom have financial connections with pharmaceutical companies), and their judgements have to be based on information presented by the pharmaceutical companies. This is pretty much an example of the fox guarding the hen house, and one has to wonder if anyone is actually looking out for the interests of the consumers/patients.
Thanks for the link. It's good to see a post from you, and I hope that you're feeling better these days.
Love,
Wayne
As far as I'm aware, that's the first that we've seen about Entyvio (vedolizumab) on this discussion board. It's apparently a new class of drugs, as far as treating IBDs is concerned (it's an integrin receptor antagonist). It will be interesting to see how it fares in actual use.
IMO, the FDA should have waited before releasing it for use, based on their obvious concerns about the possible risk of patients developing progressive multifocal leukoencephalopathy (PML). Call me old-fashioned, but I believe that the FDA should be required to make sure that all trials are completed before a drug is released for sale, whenever there is a reason to suspect that a significant risk of adverse events exists. Apparently they chose to allow patients who receive prescriptions for the drug to be used as guinea pigs for determining or ruling out any risk of developing PML. That's clear in the FDA's requirement that the drug maker "must conduct a post-approval study to further investigate the risk of PML among patients taking Entyvio".
That said, this certainly isn't the first time that the FDA has approved a drug before the extent of risks have been verified by trials. They don't actually perform any tests themselves. Instead, they rely on the judgments of selected panel members (many/most of whom have financial connections with pharmaceutical companies), and their judgements have to be based on information presented by the pharmaceutical companies. This is pretty much an example of the fox guarding the hen house, and one has to wonder if anyone is actually looking out for the interests of the consumers/patients.
Thanks for the link. It's good to see a post from you, and I hope that you're feeling better these days.
Love,
Wayne
It is suspected that some of the hardest material known to science can be found in the skulls of GI specialists who insist that diet has nothing to do with the treatment of microscopic colitis.
- Joefnh
- Rockhopper Penguin

- Posts: 2478
- Joined: Wed Apr 21, 2010 8:25 pm
- Location: Southern New Hampshire
Tex its not only this drug, but for instance I am using Cellcept in combination with Rituximab for my Myasthenia Gravis and both are at risk for PML if you are susceptible to that virus. Along with the PML issue there is a lethality if you contract the JC (John Cunningham) virus while on either of the 2 meds. When entering this arena its not to be taken lightly and there better be good reason to need to take these risks. I can understand these choices though, at the moment I am in the ICU at a local hospital in NH this week fighting issues with MG & just being able to keep breathing and I can understand why its possible to assume these risks when faced with certain challenges.
Bottom line, for certain conditions no easy answers. Personally for an IBD I would think twice about these types of treatments as there are far better options such as following a Gf, DF & SF diet which for many brings control if not remmision from MC.
Bottom line, for certain conditions no easy answers. Personally for an IBD I would think twice about these types of treatments as there are far better options such as following a Gf, DF & SF diet which for many brings control if not remmision from MC.
Joe
Joe,
Man, I'm sorry to hear that you're having those problems. I hear you. And I hope that you and the hospital staff can get those issues back under control soon.
Tex
Man, I'm sorry to hear that you're having those problems. I hear you. And I hope that you and the hospital staff can get those issues back under control soon.
Tex
It is suspected that some of the hardest material known to science can be found in the skulls of GI specialists who insist that diet has nothing to do with the treatment of microscopic colitis.
Joe,
I too have Myasthenia Gravis. Dx'd a year ago. Two ICU visits and hospital stays with Myasthenic crisis's later, and Pregnisone I have only mildly flared since.
I am so sorry you are in the hospital. I hope you are out soon. Once the mysthenic crisis was over/controlled, I always left in worse shape than when arriving. Hope you can rest and recover at home soon.
I was dx'd with LC in April 2014. Full on symptoms came in suddenly in Jan 2014. I strongly suspect my MG and LC are related. I have been suffering from head drop in the last month, and some walking difficulties. As the LC gets worse (Mast cell involvement), my MG symptoms grow. Visual disturbances, Ptosis, MG fatigue grow.
Curious if you think there has been any relation for you between the two?
I'm in Boston. Beth-Israel neuromuscular clinic, and some Mass General docs. Neurologists and Gi's don't really talk, so tough to know what's what sometimes. I'm waiting for my July (hopefully moved up) appointment with Dr. Matthew Williams at Brigham and Women's Mastocystitis Clinic. Trying to stay off Pregnisone till then. Thanks for great information on CellCept and other similiar drugs. Wow, much to think about! -Chris
I too have Myasthenia Gravis. Dx'd a year ago. Two ICU visits and hospital stays with Myasthenic crisis's later, and Pregnisone I have only mildly flared since.
I am so sorry you are in the hospital. I hope you are out soon. Once the mysthenic crisis was over/controlled, I always left in worse shape than when arriving. Hope you can rest and recover at home soon.
I was dx'd with LC in April 2014. Full on symptoms came in suddenly in Jan 2014. I strongly suspect my MG and LC are related. I have been suffering from head drop in the last month, and some walking difficulties. As the LC gets worse (Mast cell involvement), my MG symptoms grow. Visual disturbances, Ptosis, MG fatigue grow.
Curious if you think there has been any relation for you between the two?
I'm in Boston. Beth-Israel neuromuscular clinic, and some Mass General docs. Neurologists and Gi's don't really talk, so tough to know what's what sometimes. I'm waiting for my July (hopefully moved up) appointment with Dr. Matthew Williams at Brigham and Women's Mastocystitis Clinic. Trying to stay off Pregnisone till then. Thanks for great information on CellCept and other similiar drugs. Wow, much to think about! -Chris
Diagnosed April 2014, after losing 50 lbs. in 6 months.
Delzicol April 2014 (no effect, after 3.5 weeks-removed)
Endicort April 2014 - helping, but still losing.
Pepto-Bismal 9 a day - May 2014
Thankful for support!
Delzicol April 2014 (no effect, after 3.5 weeks-removed)
Endicort April 2014 - helping, but still losing.
Pepto-Bismal 9 a day - May 2014
Thankful for support!
- Joefnh
- Rockhopper Penguin

- Posts: 2478
- Joined: Wed Apr 21, 2010 8:25 pm
- Location: Southern New Hampshire
Thanks Tex, the staff here seems pretty good and do a great job with dietary intolerances. So far it looks like I can get out of here by Friday, possibly earlier.
Hello Jean, how is the new home? Hopefully the unpacking went well, thats always the 'fun' part. What about Theo, any new friends? You know its not smooth right now and is what it is...a bumpy ride. One thing about bumpy rides, they make us appreciate the smooth ones that much more :-) If all goes well I should be able to break out of here by the weekend With some tweaks to meds I am feeling better, they are just running a lot of tests. One thing I hate about ICU I have 22 wires hooked to various bits of me making it awful hard to make it to the bathroom ...Now I now what my experiments at work feel like LOL
...Now I now what my experiments at work feel like LOL
Hello Chris fellow MC & MG'r thats a rare statistical find. Chris I am up in Manchester N.H. and I work for MIT both on campus and at their Hanscom AFB facility in Lexington. Along with my local neurologist here in Manchester I also visit the group over at Mass General, Dr David, Dr Guidon and Dr Lowery. That group did all of my SFEMG and EMG testing (all tets came back positive)
A quick history: About 4 years ago I was Dx'd with both Crohn's and MC (CC) and put on Imuran. At that time no signs of Myasthenia Gravis (MG). In the summer of 2012 I started getting some random mild symptoms that I would later learn were MG, loss of voice, swallowing problems, double vision, speech problems, body wide weakness and breathing issues. About a year ago these symptoms went from random to more or less full time. At this time we started the 5 day series IVIG infusions which I continue to recieve on a as needed basis through a surgically implanted port-a-cath cardiac central line.
This past September I noticed that the Imuran was not controlling my MC or Crohns that well. By early winter we decided to try Rituximab initially and then with methotrexate for a time. That worked to a degree but also really pushed my blood levels too low. Just a few months ago we decided to add Cellcept to the Rituximab in place of the methotrexate and so far that appears to be helping quite a bit although we are still slowly increasing the dosages.
As far as a relationship between the MG & MC there is certainly one. I have found that the Cellcept does a great job of helping the MG, MC and the Crohn's, the Rituximab seems to manage the MG only. When the MG is flaring up so is the MC. As they are both autoimmune that makes sense
Chris are you familiar with the website Daily Strength and the NH / Mass MG support group? They meet every other month at the Newton Wesley Hospital.
MG Support Group Organizations:
http://www.ma-nhmgfa.org/Massachusetts_ ... lcome.html
https://www.facebook.com/MA.NH.Chapter
MG Online support group:
http://www.dailystrength.org/c/Myasthen ... port-group
Hello Jean, how is the new home? Hopefully the unpacking went well, thats always the 'fun' part. What about Theo, any new friends? You know its not smooth right now and is what it is...a bumpy ride. One thing about bumpy rides, they make us appreciate the smooth ones that much more :-) If all goes well I should be able to break out of here by the weekend With some tweaks to meds I am feeling better, they are just running a lot of tests. One thing I hate about ICU I have 22 wires hooked to various bits of me making it awful hard to make it to the bathroom
Hello Chris fellow MC & MG'r thats a rare statistical find. Chris I am up in Manchester N.H. and I work for MIT both on campus and at their Hanscom AFB facility in Lexington. Along with my local neurologist here in Manchester I also visit the group over at Mass General, Dr David, Dr Guidon and Dr Lowery. That group did all of my SFEMG and EMG testing (all tets came back positive)
A quick history: About 4 years ago I was Dx'd with both Crohn's and MC (CC) and put on Imuran. At that time no signs of Myasthenia Gravis (MG). In the summer of 2012 I started getting some random mild symptoms that I would later learn were MG, loss of voice, swallowing problems, double vision, speech problems, body wide weakness and breathing issues. About a year ago these symptoms went from random to more or less full time. At this time we started the 5 day series IVIG infusions which I continue to recieve on a as needed basis through a surgically implanted port-a-cath cardiac central line.
This past September I noticed that the Imuran was not controlling my MC or Crohns that well. By early winter we decided to try Rituximab initially and then with methotrexate for a time. That worked to a degree but also really pushed my blood levels too low. Just a few months ago we decided to add Cellcept to the Rituximab in place of the methotrexate and so far that appears to be helping quite a bit although we are still slowly increasing the dosages.
As far as a relationship between the MG & MC there is certainly one. I have found that the Cellcept does a great job of helping the MG, MC and the Crohn's, the Rituximab seems to manage the MG only. When the MG is flaring up so is the MC. As they are both autoimmune that makes sense
Chris are you familiar with the website Daily Strength and the NH / Mass MG support group? They meet every other month at the Newton Wesley Hospital.
MG Support Group Organizations:
http://www.ma-nhmgfa.org/Massachusetts_ ... lcome.html
https://www.facebook.com/MA.NH.Chapter
MG Online support group:
http://www.dailystrength.org/c/Myasthen ... port-group
Joe
Joe,
That's definitely good news that you'll be out of there by tomorrow.
Quick question — has any doctor ever tested your tryptase level soon after an MG flare begins? IOW, have they ever done a test early enough in the flare to catch your tryptase level in an elevated state (in the event that mastocytosis might be playing a part in triggering the flares).
Tex
That's definitely good news that you'll be out of there by tomorrow.
Quick question — has any doctor ever tested your tryptase level soon after an MG flare begins? IOW, have they ever done a test early enough in the flare to catch your tryptase level in an elevated state (in the event that mastocytosis might be playing a part in triggering the flares).
Tex
It is suspected that some of the hardest material known to science can be found in the skulls of GI specialists who insist that diet has nothing to do with the treatment of microscopic colitis.
- Joefnh
- Rockhopper Penguin

- Posts: 2478
- Joined: Wed Apr 21, 2010 8:25 pm
- Location: Southern New Hampshire
Tex I do not believe they have measured the tryptase levels during a period of disease activity. Is there an association between tryptase and acetylcholine or acetylcholine estrace??
As a side note, many get quickly confused as to the mechanism of action that causes a breathing crisis in MG. It is not the contraction of the smooth muscle tissue causing an airway restriction, the airway is not affected by MG and the airway is generally clear and fully open during a crisis. The cause of a MG crisis is muscle fatigue of the striated muscles that make up the diaphragm, and accessory muscle groups that actually are responsible for inflating and deflating the lungs themselves. These muscles are weakened and unable to function resulting in the inability to move air in and out of the lungs.
When the acetylcholine receptors on those muscles are damaged or clogged up by the MG ACHR antibodies caused by the autoimmune process they lose strength and fatigue easily eventually resulting in the muscle no longer able to do its job .... breathing, thats when the fun begins
Essentially Tex with MG any striated muscle which is muscle you can voluntarily move, is at risk of significant fatiguable weakness, long term receptor damage and some degree of long term paralysis if the progression of MG is left untreated
As a side note, many get quickly confused as to the mechanism of action that causes a breathing crisis in MG. It is not the contraction of the smooth muscle tissue causing an airway restriction, the airway is not affected by MG and the airway is generally clear and fully open during a crisis. The cause of a MG crisis is muscle fatigue of the striated muscles that make up the diaphragm, and accessory muscle groups that actually are responsible for inflating and deflating the lungs themselves. These muscles are weakened and unable to function resulting in the inability to move air in and out of the lungs.
When the acetylcholine receptors on those muscles are damaged or clogged up by the MG ACHR antibodies caused by the autoimmune process they lose strength and fatigue easily eventually resulting in the muscle no longer able to do its job .... breathing, thats when the fun begins
Essentially Tex with MG any striated muscle which is muscle you can voluntarily move, is at risk of significant fatiguable weakness, long term receptor damage and some degree of long term paralysis if the progression of MG is left untreated
Joe
Joe and Tex,
I watched Dr. Cassell's video on Vimeo about their work at the Mastocystitis center at Brigham's. Interesting acetylcholine mention at one point, along with sympathetic and parasympyhetic neurological weaknesses.
My memory (possibly Mast cell involvement, as short-term memory loss, and Brain fog, is the most commonly reported symptom) is having a hard time putting some of this together. So as I research, I grab onto bits and pieces like acetylcholine mention, I forget or I'm unable to follow through. So sorry for sketchy info. But, please keep in mind as you research.
Joe, I agree. MG is it's own autoimmune with specific blood antibody markers, and very unique symptoms caused by acetylcholine receptor sites, "being clogged." But, AI diseases often come in groups. I find it interesting that some of the symptoms of Mast cell involvement in MC, shares some of the same symptoms. Hard to know which is caused by what. For me it was MG first, then MC.
Joe, I did the MG walk last year at Chestnut Hill Resovior. I could not walk well,as I was recovering from major flare. Were you there? I have not gone to the support group meetings yet, always seems like something comes up, or I am too fatigued. I also have been in a fairly full remission for almost a year (minus the MC onset in Jan), and often just want to forget MG. I know, a very selfish attitude, as I need support, as well as be willing to help others, and not live in isolation.
I have seen Dr. David at MGH. Love him. If I seriously flare, and need to consider more serious drug therapy, or a return to Pregnisone, I believe I will choose Dr. David and the MGH neuromuscular clinic as my primary Neuro's. I have 5 separate Neuro's now, and it has gotten to be a mess, over at BI. I like the fact that Dr. David, considers all my issues and doesn't just refer me out. My only hesitation, is he requires me to have another SFEMG done by him. I've already done two. Very painful for me as I also have trigeminal neurolgia, and I show the most conclusive SFEMG results around my eye. I just can't fathom doing this again. At least until I'm stronger.
Enough MG talk, over here on an MC forum:) so good to have a fellow traveler. Hope you are out if the hospital today!!!!!!
I watched Dr. Cassell's video on Vimeo about their work at the Mastocystitis center at Brigham's. Interesting acetylcholine mention at one point, along with sympathetic and parasympyhetic neurological weaknesses.
My memory (possibly Mast cell involvement, as short-term memory loss, and Brain fog, is the most commonly reported symptom) is having a hard time putting some of this together. So as I research, I grab onto bits and pieces like acetylcholine mention, I forget or I'm unable to follow through. So sorry for sketchy info. But, please keep in mind as you research.
Joe, I agree. MG is it's own autoimmune with specific blood antibody markers, and very unique symptoms caused by acetylcholine receptor sites, "being clogged." But, AI diseases often come in groups. I find it interesting that some of the symptoms of Mast cell involvement in MC, shares some of the same symptoms. Hard to know which is caused by what. For me it was MG first, then MC.
Joe, I did the MG walk last year at Chestnut Hill Resovior. I could not walk well,as I was recovering from major flare. Were you there? I have not gone to the support group meetings yet, always seems like something comes up, or I am too fatigued. I also have been in a fairly full remission for almost a year (minus the MC onset in Jan), and often just want to forget MG. I know, a very selfish attitude, as I need support, as well as be willing to help others, and not live in isolation.
I have seen Dr. David at MGH. Love him. If I seriously flare, and need to consider more serious drug therapy, or a return to Pregnisone, I believe I will choose Dr. David and the MGH neuromuscular clinic as my primary Neuro's. I have 5 separate Neuro's now, and it has gotten to be a mess, over at BI. I like the fact that Dr. David, considers all my issues and doesn't just refer me out. My only hesitation, is he requires me to have another SFEMG done by him. I've already done two. Very painful for me as I also have trigeminal neurolgia, and I show the most conclusive SFEMG results around my eye. I just can't fathom doing this again. At least until I'm stronger.
Enough MG talk, over here on an MC forum:) so good to have a fellow traveler. Hope you are out if the hospital today!!!!!!
Diagnosed April 2014, after losing 50 lbs. in 6 months.
Delzicol April 2014 (no effect, after 3.5 weeks-removed)
Endicort April 2014 - helping, but still losing.
Pepto-Bismal 9 a day - May 2014
Thankful for support!
Delzicol April 2014 (no effect, after 3.5 weeks-removed)
Endicort April 2014 - helping, but still losing.
Pepto-Bismal 9 a day - May 2014
Thankful for support!
There is no association between tryptase and either of those items that I'm aware of, except for the secondary association described in the rest of this paragraph. You're probably well aware of this association, but I'll describe it here for the benefit of anyone who is not familiar with it. The serum tryptase level is the only practical way (that I'm aware of) to monitor mast cell activity. IOW, when mast cells degranulate to release histamine, cytokines, and other pro-inflammatory agents, they also release the tryptase enzyme. The elevation in serum tryptase levels approximates the increase of histamine and other pro-inflammatory mediators. About 2 hours after a mast cell activation event, serym tryptase levels peak, and then slowly decline. Therefore the blood draw must be done within a few hours of the initiation of the degranulation event, in order to show an elevated result.Joe wrote:Is there an association between tryptase and acetylcholine or acetylcholine estrace??
Mast cells are almost surely directly involved in virtually all reactions associated with autoimmune issues. This is strictly my opinion, but evidence certainly exists to suggest that this is also the case with MG. Consider these old research articles:
Characteristics of histamine release evoked by acetylcholine in isolated rat mast cells.
Immunological modulation of cholinergic histamine release in isolated rat mast cells
Nicotinic acetylcholine receptors on basophils and mast cells.
But my point is that mast cells are definitely associated with the expression of acetylcholinesterase.
Murine and human mast cell express acetylcholinesterase
This should give you a basis that you can use as a springboard for additional research. But remember that in the presence of immune system suppression, the basic rules that govern these reactions may be modified or suppressed (possibly in unpredictable ways in some cases), so that otherwise predictable associations and reactions may become more complex, and therefore possibly unpredictable.
Exactly! And if you think about this, what causes fatigue (ultimately)? As we are so well aware, as MC hosts, the answer is (IMO) "inflammation". And what causes inflammation? In the vast majority of cases, either T-cell infiltration (in the case of epithelial tissues), or mast cell activity (in most other soft tissue). Yes, there are many other inflammation modulators, but with the AI issues that we typically have to deal with, T-cells and mast cells are the big dogs in the fight. Since the diaphragm is not epithelial tissue, then mast cells are the most likely engine of inflammation in that situation.Joe wrote:The cause of a MG crisis is muscle fatigue of the striated muscles that make up the diaphragm, and accessory muscle groups that actually are responsible for inflating and deflating the lungs themselves. These muscles are weakened and unable to function resulting in the inability to move air in and out of the lungs.
At the moment, I have no idea how the details of this process might play out, but I definitely agree with Chris that mast cells are a major player in the issues that you are dealing with. IOW I'm convinced that some form of mast cell activation disorder is associated with MG (and responsible for many/most of the most damaging symptoms). It might turn out to be a secondary issue, but even if it is secondary, it's still a powerful effect, and one about which very little is known, making these waters murky, and uncharted.
Tex
It is suspected that some of the hardest material known to science can be found in the skulls of GI specialists who insist that diet has nothing to do with the treatment of microscopic colitis.
- Joefnh
- Rockhopper Penguin

- Posts: 2478
- Joined: Wed Apr 21, 2010 8:25 pm
- Location: Southern New Hampshire
Tex the etiology of MG is not due to inflammation, more so it is the AcHR antibodies attacking the receptors and the neuromuscular level. This issue has been fully understood since the 1920's and has been treated even at that early date with cortisol and Pyrodistimine Bromide (Mestinon)
Lets take a moment and review the mechanisms involved in the autoimmune condition. Here is a write up done by Yale Medical that outlines MG fairly well.
Pathophysiology
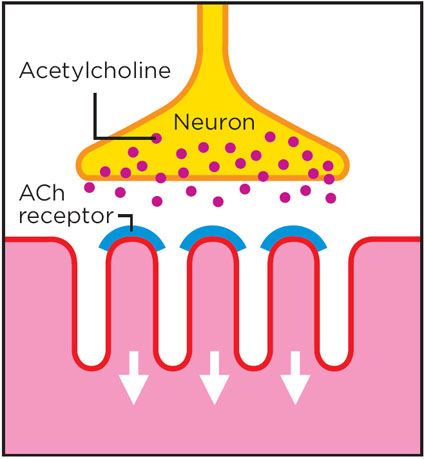
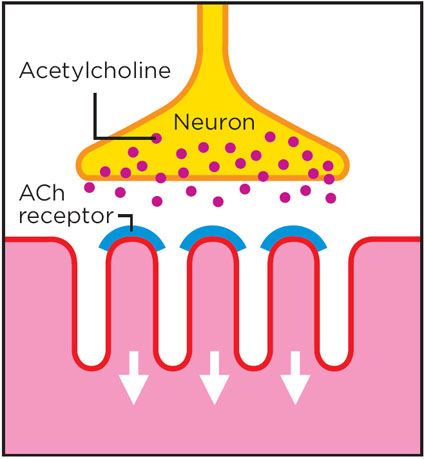
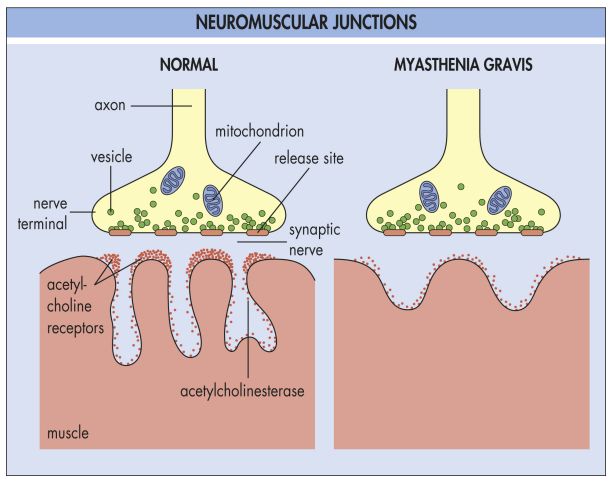
Myasthenia gravis is a disorder of neuromuscular transmission. In order to understand what causes MG, we must first describe what constitutes normal neuromuscular transmission.
Normal Neuromuscular Transmission
Acetylcholine (ACh) is synthesized in the nerve terminal by action of the enzyme choline acetyltransferase. ACh is then stored in vesicles, forming a quantum, containing about 10,000 molecules of ACh. Quanta of ACh are released into the nerve terminal by calcium dependent exocytosis - the fusing of the vesicles with the outer membrane wall. ACh then binds to the post-synaptic ACh receptor, resulting in a transient increase in membrane permeability to Na, K, Ca, and Mg, leading to an Endplate potential (EPP). Spacial and temporal summation of the EPPís are usually sufficient to reach threshold and cause a muscle membrane action potential. Acetycholinesterase and diffusion deactivates the ACh and terminates neuromuscular transmission.
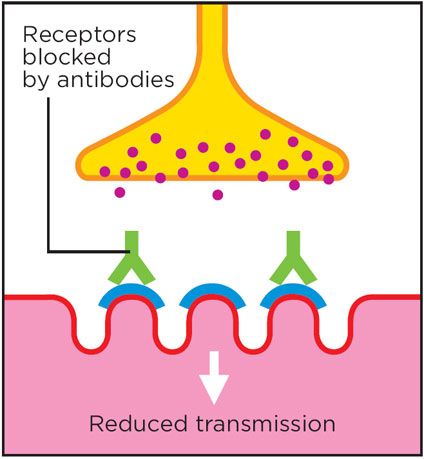
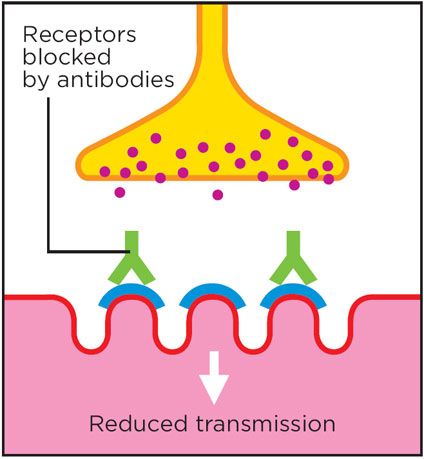
Acetylcholine Receptor Antibody
The culprit in MG is an abnormally created antibody which has activity against the acetylcholine receptor, which is why MG is classified as an autoimmune disease. The AChR antibody is polyclonal and is present in 85-95% of MG cases. The antibody blocks neuromuscular transmission by several mechanisms - blockade of receptor sites by steric hindrance, destruction of AChR (complement mediated), and crosslinking of AChR which causes increased turnover by endocytosis (from 5-6 days to 2.5 days).
These effects collectively decrease the number of acetylcholine molecules binding to receptors, therefore decreasing the number of EPP's, and decreasing the likelihood of the muscle fiber reaching threshold depolarization and contracting. The resulting decrease in the number of muscle fibers firing is what causes weakness.
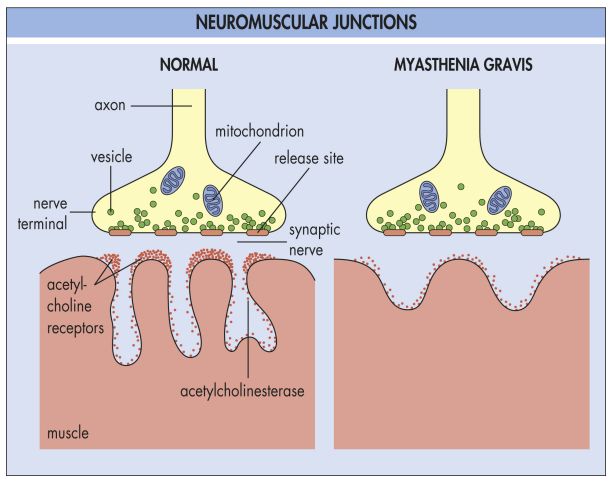
Structural Changes
The chronic inflammation of MG causes several changes in the structure of the Neuromuscular Junction which also inhibit transmission and contribute to weakness. These include flattening out of the junctional folds, spreading out of AChR and Acetylcholinesterase, a 66% decrease in number of AChR, and an increased junctional gap.
Normal Neuromuscular Interface:
Neuromuscular Interface Affected by AcHR Antibodies
Another Example Image. Notice the damage in the muscle with the reduced number of folds and receptors (Right). This damage does become permanent if not treated correctly resulting in partial or complete paralysis of that muscle
When I look at your statement:
From what I can tell from the articles you referenced there is no inflammatory response involved with the weakening of the striated muscles. Maybe I missed those references.
Lets take a moment and review the mechanisms involved in the autoimmune condition. Here is a write up done by Yale Medical that outlines MG fairly well.
Pathophysiology
Myasthenia gravis is a disorder of neuromuscular transmission. In order to understand what causes MG, we must first describe what constitutes normal neuromuscular transmission.
Normal Neuromuscular Transmission
Acetylcholine (ACh) is synthesized in the nerve terminal by action of the enzyme choline acetyltransferase. ACh is then stored in vesicles, forming a quantum, containing about 10,000 molecules of ACh. Quanta of ACh are released into the nerve terminal by calcium dependent exocytosis - the fusing of the vesicles with the outer membrane wall. ACh then binds to the post-synaptic ACh receptor, resulting in a transient increase in membrane permeability to Na, K, Ca, and Mg, leading to an Endplate potential (EPP). Spacial and temporal summation of the EPPís are usually sufficient to reach threshold and cause a muscle membrane action potential. Acetycholinesterase and diffusion deactivates the ACh and terminates neuromuscular transmission.
Acetylcholine Receptor Antibody
The culprit in MG is an abnormally created antibody which has activity against the acetylcholine receptor, which is why MG is classified as an autoimmune disease. The AChR antibody is polyclonal and is present in 85-95% of MG cases. The antibody blocks neuromuscular transmission by several mechanisms - blockade of receptor sites by steric hindrance, destruction of AChR (complement mediated), and crosslinking of AChR which causes increased turnover by endocytosis (from 5-6 days to 2.5 days).
These effects collectively decrease the number of acetylcholine molecules binding to receptors, therefore decreasing the number of EPP's, and decreasing the likelihood of the muscle fiber reaching threshold depolarization and contracting. The resulting decrease in the number of muscle fibers firing is what causes weakness.
Structural Changes
The chronic inflammation of MG causes several changes in the structure of the Neuromuscular Junction which also inhibit transmission and contribute to weakness. These include flattening out of the junctional folds, spreading out of AChR and Acetylcholinesterase, a 66% decrease in number of AChR, and an increased junctional gap.
Normal Neuromuscular Interface:
Neuromuscular Interface Affected by AcHR Antibodies
Another Example Image. Notice the damage in the muscle with the reduced number of folds and receptors (Right). This damage does become permanent if not treated correctly resulting in partial or complete paralysis of that muscle
When I look at your statement:
Inclusing the supporting documents, the descriptors used there as the precursors for acetylcholine esterase are referring to smooth muscle involvement, not striated muscle involvement. This makes sense as we know that for instance those asthma for instance are affected mast cell activation as the mast cell activity results in changes to the smooth muscle structured in the lungs resulting in wheezing and other constrictive airway issues. With MG,constrictive airway is not involved, just the striated muscles involved with the diaphragm and accessory muscles when it comes to being able to breathe.Mast cells are almost surely directly involved in virtually all reactions associated with autoimmune issues. This is strictly my opinion, but evidence certainly exists to suggest that this is also the case with MG. Consider these old research articles:
From what I can tell from the articles you referenced there is no inflammatory response involved with the weakening of the striated muscles. Maybe I missed those references.
Joe
- Tessa
- Rockhopper Penguin

- Posts: 774
- Joined: Thu May 26, 2005 2:49 pm
- Location: Málaga, Spain (Costa del Sol)
- Contact:
Thank you, Tex. 
I am still having health problems. Some days I am in bed for about 13 hours to recover because I feel exhausted... But I am trying to cope with it...
I am with you, FDA should have waited before releasing it for use. This is not a game. But they are playing with our health.
Risks should be verified before releasing a new drug. Trials are there for it and not us to become their way to try a new drug.
Thank you.
Love,
Tessa
I am still having health problems. Some days I am in bed for about 13 hours to recover because I feel exhausted... But I am trying to cope with it...
I am with you, FDA should have waited before releasing it for use. This is not a game. But they are playing with our health.
Risks should be verified before releasing a new drug. Trials are there for it and not us to become their way to try a new drug.
Thank you.
Love,
Tessa
DX Secondary Adrenal Insufficiency= Panhypopituitarism,POTS & MC. Anaphylactic reaction to foods & some drugs.
Gluten & Dairy free diet+hydrocortisone, Florinef, Sea Salt, Vit B Complex, Potassium, Sodium, Magnesium...
Gluten & Dairy free diet+hydrocortisone, Florinef, Sea Salt, Vit B Complex, Potassium, Sodium, Magnesium...

