I have come to wonder how is it that now that we are 100% GF,DF and SF. We have identified our reactive foods even through MRT testing, yet we still have some symptoms. So the question is what else is contributing to these symptoms that we may have been attributing to MC.
What started this was some research I began after taking with Gabes about how well she tolerated both the local anasthetics used in dental work and anasthetics used during a colonoscopy. In both cases Gabes had significantly exacerbated MC and other systemic affects from the administration of those compounds, a rare reaction
In particular the intolerance to the local anasthetics is quite rare and is a possible indicator of eithier histamine intolerance or a mast cell reaction. Similar to Gabes, I have noticed that I do not tolerate some of the narcotic based pain medications used after surgery particularly morphine which was given to me during the last 2 surgeries.
In both of our cases we have noted that these medication intolerances and general allergy symptoms have gotten worse after we had gained control of MC through diet alone and in my case diet and meds. This seemed strange as we have been eliminating our problem foods and it would seem we would have less allergy symptoms. In one of our conversations we have wondered if this is a similar or related pattern, that several members here have reported as additional food intolerances that seem to crop up one after another over time. It was this thought that launched this bit of research
After a great deal of research I have come to a possible conclusion that the affects of elevated levels of histamine and/or an intolerance to histamine most likely exacerbates the GI symtoms we have with MC.
This article from the American Journal of Clinical Nutrition presented one of the best papers on this topic.
http://www.ajcn.org/content/85/5/1185.full
Within the full text link you can select from above there is a good summary of the medications which seem to play a role in the release of histamine that potentially causes the GI symptoms listed aboveHistamine and headache
Headache can be induced dose-dependently by histamine in healthy persons as well as in patients with migraine (53, 61). Histamine-induced headache is a vascular headache caused mainly by nitrate monoxidase
Histamine and gastrointestinum
Besides headache, gastrointestinal ailments including diffuse stomach ache, colic, flatulence, and diarrhea are leading symptoms of histamine intolerance. Elevated histamine concentrations and diminished DAO activities have been shown for various inflammatory and neoplastic diseases such as Crohn disease (17), ulcerative colitis (67), allergic enteropathy (39), food allergy (33, 68, 69), and colorectal neoplasmas (24). In the colonic mucosa of patients with food allergy, a concomitant reduced HNMT (70) and an impaired total histamine degradation capacity (THDC) (69) have been found (33), so that the enzymes cannot compensate each other. Therefore, an impaired histamine metabolism has been suggested to play a role in the pathogenesis of these diseases.
As far as personal experience, I have found that I cannot tolerate morphine or amitriptyline. Prior to my diagnosis of MC and Crohns I was put on Elavil (amitriptyline) to help deal with cramps and muscle & joint pains that I now realize was most likely gluten and other dietary intolerances. I did note that the Elavil did make my cramps actually worse and caused an increase in mucosal production in my sinuses. Here Gabes also has had a reaction to the use of prilocaine as a local anasthetic during dental work.
TABLE 5 Drugs releasing histamine or inhibiting diamine oxidase
Substance class Agent interfering with the histamine metabolism
Contrast media: Pancuronium, alcuronium, D-tubocurarine
Muscle relaxants : Thiopental
Narcotics
Analgetics: Morphine, pethidine, nonsteroidal antiinflammatory drugs,
acetylsalicylic acid, metamizole
Local anesthetics: Prilocaine
Antihypotonics: Dobutamine
Antihypertensive drugs: Verapamil, alprenolol,
Antiarrhythmics: Propafenone
Diuretics: Amiloride
Drugs influencing gut motility: Metoclopramide
Antibiotics: Cefuroxime, cefotiam, isoniazid, pentamidin, clavulanic acid, choroquine
Mucolytics: Acetylcysteine, ambroxol
Broncholytics: Aminophylline
H2-receptor antagonists: Cimetidine
Cytostatics: Cyclophosphamide
Antidepressants: Amitriptyline
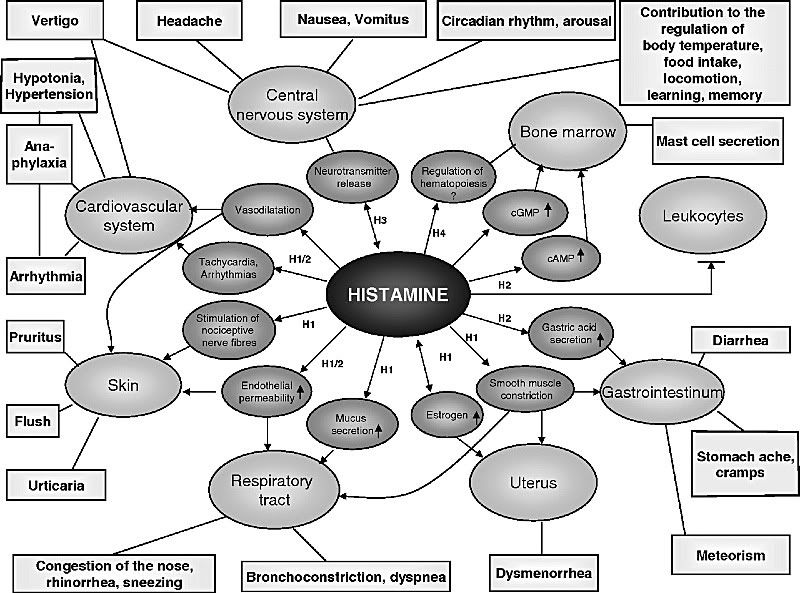
The effects of histamine on our bodies is far reaching and does have several of the same features that are noted with IBDs including MC which include cramping, D, meteorism and nausea. In relation to the same article listed above, here is a good chart which shows the affects H1,H2,H3 or H4 histamine release has and their related symptoms.
So whether it is due to mast cell disease or a more general release of histamine, overall it does seem that histamine plays a key role in our symptoms of which many are the same in both MC or high levels of histamine.
As a part of this research Gabes and I have been performing a trial of antihistamine therapy for the past week, and have had some surprising results. For the trial we both have been taking 10mg of Claritin (Loratedine) in the AM and between 12 to 25 mg of Benadryl (diphenhydramine) at night.
After about the fourth day I have noticed significantly improved stool formation (all normans), vastly improved energy, clearer mind (less brain fog) and overall a better sense of just feeling well. I thought I was doing pretty well before this especially compared to how I was doing when MC first really kicked in, but I can see now that there was still room for improvement. Gabes also has begun to see improvements in some of her symptoms, I'll let her update her progress as she has a differrent list of symptoms that she deals with that is also strikingly similar to the chart shown above.
I'm hoping Tex can weigh in here on this.... I have a theory that in systemic and chronic histamine release, increased mucosal production is seen throughout the mucosal membranes which include the GI tract. Is it possible that a chronic release of mucous, or the chronic presence of histamine in the GI tissues to result in the buildup of lymphocytes in the mucosal layers of the tissues that make up the GI tract?
I will be continuing to look into this topic, but can't help to wonder if for many of us if histamine is playing an aggravating role in MC, complicating our symptoms and potentially playing a role in the development of new food intolerances. As a thought is this why the MRT testing and related avoidance of the highly reactive foods is so successful in some of us? While I'm not sure of this the MRT testing is based on (IgE ?) level testing which is generally used for determining allergic reactions, an avoidance of the highly reactive foods would lower the histamine levels we experince daily.
Joe



